Reducing Fall Risk in the Aging IDD Population
As individuals with intellectual and developmental disabilities (I/DD) age, they face unique challenges that require specialized attention, particularly when it comes to managing fall risks. This growing demographic, living longer and healthier lives, now mirrors the general population in life expectancy. However, they are more likely to develop chronic health conditions earlier, leading to an increased risk of falls—a concern that demands a multidisciplinary approach to prevention and care.
The Aging Population and Increased Fall Risk
The aging population of individuals with I/DD is expanding rapidly. The number of adults aged 60 and older with developmental disabilities is expected to nearly double to 1.2 million by 2030. This demographic shift introduces fresh challenges for healthcare providers, as these individuals are prone to developing chronic conditions earlier than the general population, including:
- Arthritis
- Type 2 diabetes
- Kidney disease
- Heart disease
- Alzheimer’s disease and other dementias
These conditions, coupled with the side effects of medications used to manage them, contribute significantly to fall risks.
Quick Facts
- 30% of adults with I/DD fall each year
- Individuals with I/DD aged 18-64 fall more often than those in the same age group across the general population
- Adults with disabilities ages 45-59 experience fall injuries at higher rates than those aged 60 and over
- Two-thirds of adults with I/DD who fall, will fall again and each fall increases the risk of a subsequent fall and more serious injury from a fall.
Falls are a serious concern because they can lead to a cascade of health issues, including fractures, loss of independence, and even death. For individuals with I/DD, the risk is even more pronounced. Research indicates that falls in this population tend to occur earlier, around the mid-50s, compared to the general population, where the risk increases significantly after age 65. This earlier onset of fall risk highlights the need for proactive management strategies tailored to the specific needs of this group.
Medication Management and Fall Risk
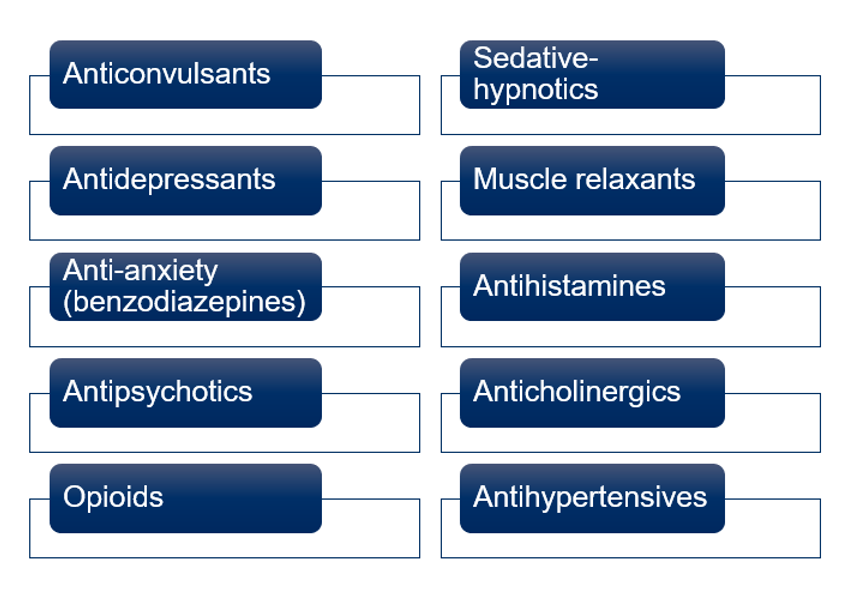
Medication is a double-edged sword in managing chronic conditions in aging populations with I/DD. While necessary for treating conditions like diabetes or heart disease, certain medications can increase the risk of falls. For example, sedatives, antidepressants, benzodiazepines, opioid analgesics, muscle relaxants, and blood pressure medications can cause drowsiness, dizziness, balance issues, and muscle weakness—all of which heighten the risk of falling. Antipsychotics can cause sedation, tremors, and extrapyramidal symptoms which increase fall risk.
Fall Risk Medications
Given these risks, medication management becomes a critical component of fall prevention. Pharmacists play a crucial role here, particularly those specializing in long-term care for individuals with I/DD. A comprehensive medication review is essential to identify drugs that may contribute to falls. Adjusting dosages, switching to less sedative alternatives, or even discontinuing unnecessary medications can significantly reduce fall risks.
Pharmacists can also work closely with other healthcare providers to ensure a holistic approach to care. This collaboration includes regular consultations, where a pharmacist might suggest alternative medications or dosages based on the individual’s overall health profile and specific risks. For instance, in the case of someone with both diabetes and a history of falls, a pharmacist might recommend blood sugar medications that are less likely to cause hypoglycemia, which can lead to falls.
Key Medication Management Strategies to Reduce Fall Risk
- Take a comprehensive medication list to every physician’s visit
- Ask the pharmacist to provide a medication regimen review to identify high fall risk medications and make recommendations to reduce risk
- Look for opportunities to discontinue or reduce the dose of high fall risk medications including psychotropics, antihypertensives, and opioid analgesics
- Medications with lower fall risk should be considered first
- Strive to find the lowest possible effective dose of high fall risk medications
- Avoid the use of psychotropic medications, when possible
- Use opioid analgesics for the shortest amount of time possible
- Reduce or discontinue sedative/hypnotic medication use, when possible, by improving sleep hygiene (e.g., reducing daytime napping, staying active throughout the day, and ensuring a cool, quiet and dark sleep environment)
- Avoid administering stimulating medications in the evening
- Evaluate medications taken within 1 to 2 hours of a fall, since they may have contributed to the fall
Environmental and Behavioral Interventions
Beyond medication management, environmental modifications and behavioral interventions are crucial in reducing fall risks. Individuals with I/DD often live in environments that may not be fully adapted to their needs as they age. Simple changes, such as removing tripping hazards, installing grab bars, and ensuring adequate lighting, can make a significant difference in preventing falls.
Behavioral factors also play a role. Encouraging regular physical activity to maintain muscle strength and balance is vital. However, fear of falling can lead to a vicious cycle where individuals become less active, further weakening their muscles and increasing fall risk. Addressing this fear through education and confidence-building exercises can help break the cycle and promote safer, more active lifestyles.
The Role of a Collaborative Care Team
Effective fall prevention requires a team approach. In addition to pharmacists, direct support professionals (DSPs), nurses, physicians, and occupational therapists all play important roles.
For example, DSPs and nurses who work closely with individuals can provide valuable insights into daily habits and potential risks, while occupational therapists can assess and modify living spaces to enhance safety.
Regular communication among team members ensures that everyone is aware of any changes in an individual’s condition or environment that could affect their fall risk. This collaborative approach not only helps prevent falls but also enhances the overall quality of life for aging individuals with I/DD.
Conclusion
The rising number of aging individuals with intellectual and developmental disabilities presents both challenges and opportunities for healthcare providers. By focusing on proactive fall risk management through medication review, environmental modifications, and a collaborative care approach, it is possible to significantly reduce the incidence of falls in this vulnerable population. Pharmacists, in particular, have a vital role in this process, offering expertise that extends beyond medication dispensing to include comprehensive fall risk assessments and personalized care strategies.
Preventing falls is not just about avoiding injuries; it’s about preserving the independence, dignity, and quality of life for aging individuals with I/DD. By working together, healthcare professionals can make a profound difference in the lives of those they serve, ensuring that they can age with the best possible health and well-being.

Curt Bicknell, Pharm.D.
President, Guardian Pharmacy Mid-South
A seasoned pharmacist and leader, Curt has more than 20-years’ experience in healthcare. He has an extensive background caring for geriatric populations including hospice clinical account management, consulting, and long-term care pharmacy services. The depth and breadth of his expertise has been a driving factor in the growth of Guardian Pharmacy Mid-South which serves long-term care communities and residents across Tennessee, Arkansas, and Mississippi. A native Memphian, Curt has spent his entire life in Memphis and is a graduate of the University of Tennessee, Memphis.








